Oxartis is glad to announce the completion of a pre-clinical study to evaluate the efficacy of our MVP, ProMatrix BioDerm. The study was conducted in collaboration with Study partner, ProDevLabs, with BridgePTS and Histology Services Ltd.
Methods
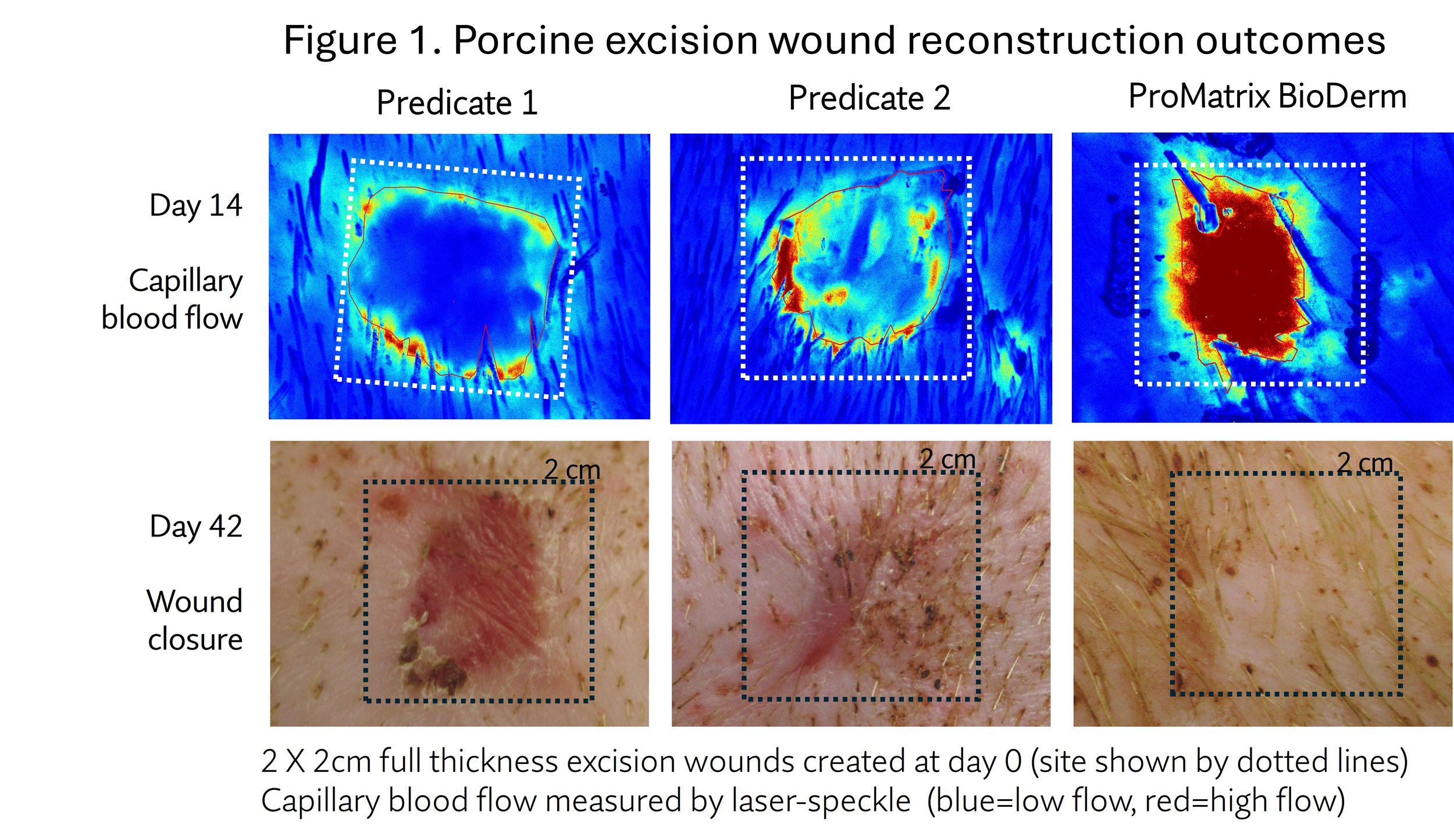
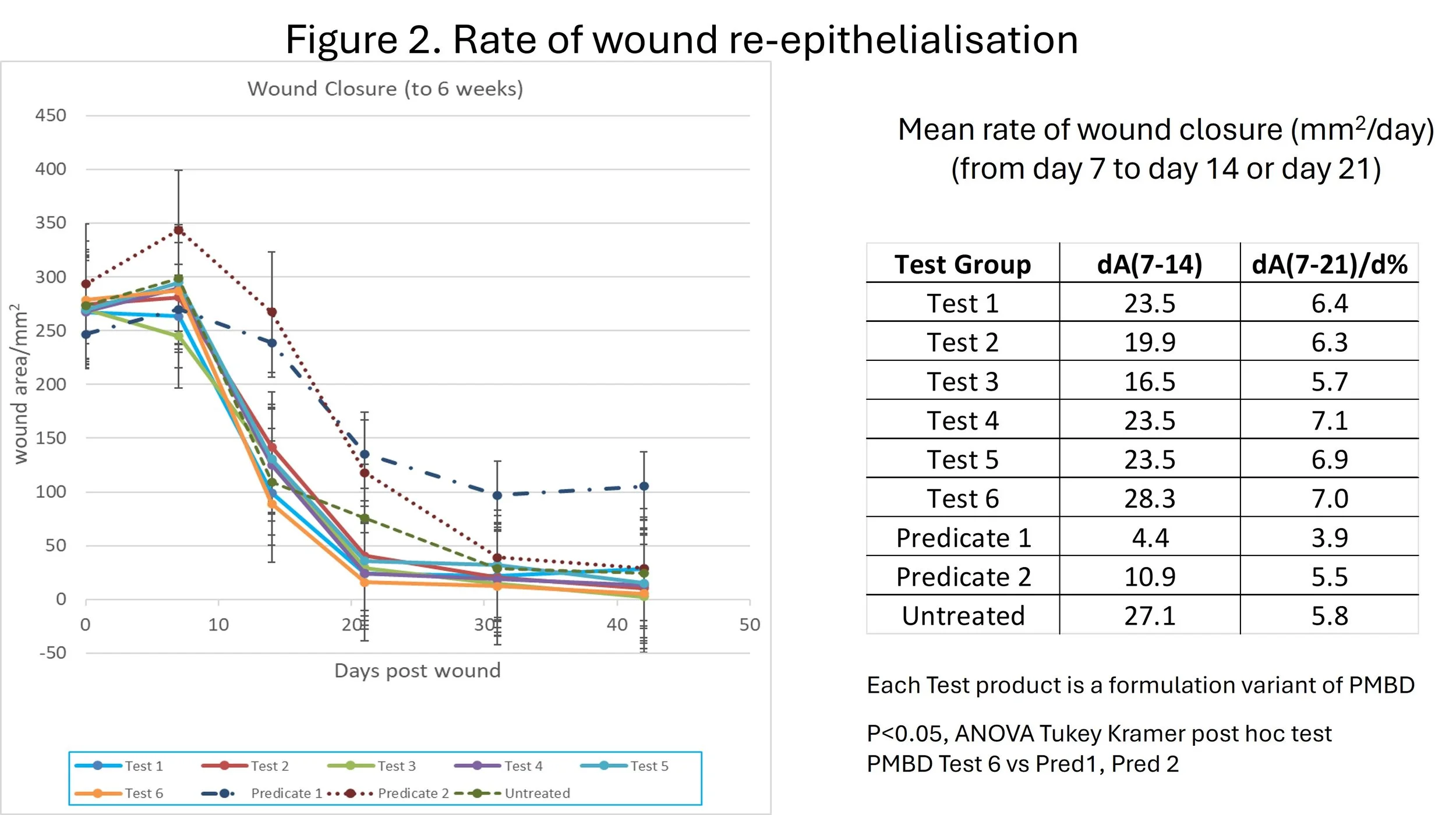
Test scaffolds were evaluated for effect on healing or reconstruction of full-thickness excision wounds in Yorkshire pigs. ProMatrix and two predicate products in widespread use globally, were evaluated side by side, together with no-scaffold control wounds, which recieved identical dressing (4 replicate wounds each treatment). All scaffolds were covered with a layer of Telfa semi-permeable plastic membrane, and bolstered with absorbent foam (Optifoam). Wounds were regularly redressed and monitored for 3 weeks by laser speckle for blood flow, sampled for histology. The study was terminated at 6 weeks, with mechanical and TEWL measurements of scar/neotissue outcome, and histology.
Results
Efficacy for dermal regenerative reconstruction (full-thickness skin excision assay, porcine in vivo, 6 weeks).
· Vascularisation into scaffolds was detected from day 3, and progressively increased to day 14. significantly greater than that achieved by competitor products.
· Epithelialisation rate (change in area/day) from day 7 to day 21, was 6 - 8 X faster than that achieved by competitor products.
· TEWL indicating accelerated 2-9 X increased skin barrier restoration at 6 weeks over that achieved by competitor products.
· Viscoelasticity of reconstructed skin significantly higher at 6 weeks over that achieved by competitor products. Specifically, neo-tissue showed 1.3-1.6 X greater elasticity and 0.6-0.74 X less viscous flow, that each competitor product.
· Histological analysis revealed that at 6 weeks, the ProMatrix neo-tissue showed dispersed collagen, without formation of dense bundles seen in scar tissue.
Conclusions
The porcine full-thickness excision wound model yielded results which gave statistically significant differences between treatment groups. The healing profile with each predicate is reflective of clinical experience. PMBD treated wounds showed rapid vascularisation into the scaffold, rapid epithelial closure over the wound neo-tissue, and tissue growth. Moreover, tracts of dense and contractile scar tissue collagen were absent from the ProMatrix neo-tissue. Therefore ProMatrix appears to support regenerative tissue reconstruction without scarring.